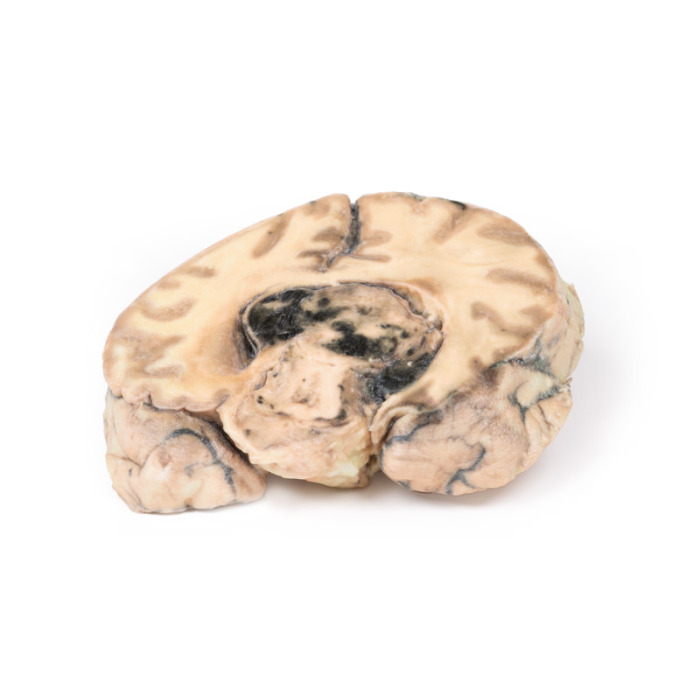
MP2016 - Glioblastoma multiforme
Clinical History
Pathology
Further Information
Gliomas are the second most common cancer of the central nervous system after meningiomas. The term “glioma” refers to tumours that are histologically similar to normal glial cells i.e. astrocytes, oligodendrocytes and ependymal cells. They arise from a progenitor cell that differentiates down one of the cell lines. Glioblastoma multiforme (GBM; also called glioblastoma) develop from the astrocyte lineage. GBMs can arise in the brain “de novo” or evolve from lower-grade astrocytomas or oligodendrogliomas. GBM is often referred to as a grade IV astrocytoma. They are differentiated histologically from anaplastic astrocytomas by necrotising tissue surrounded by anaplastic cells as well as by the presence of hyperplastic blood vessels.
GBMs are more common in males. It is most commonly diagnosed in the 6th decade of life. Genetic risk factors include neurofibromatosis type 1 and Li-Fraumeni syndrome. Previous brain radiotherapy is also associated with increased risk of GBM. Symptoms vary depending on the location of the GBM, but may include any of the following:
- Persistent headaches
- Double or blurred vision
- Vomitng
- Loss of appetite
- Changes in mood and personality
- Changes in ability to think and learn
- New onset of seizures
- Speech difficulty of gradual onset
- Quantitative unit
- ks
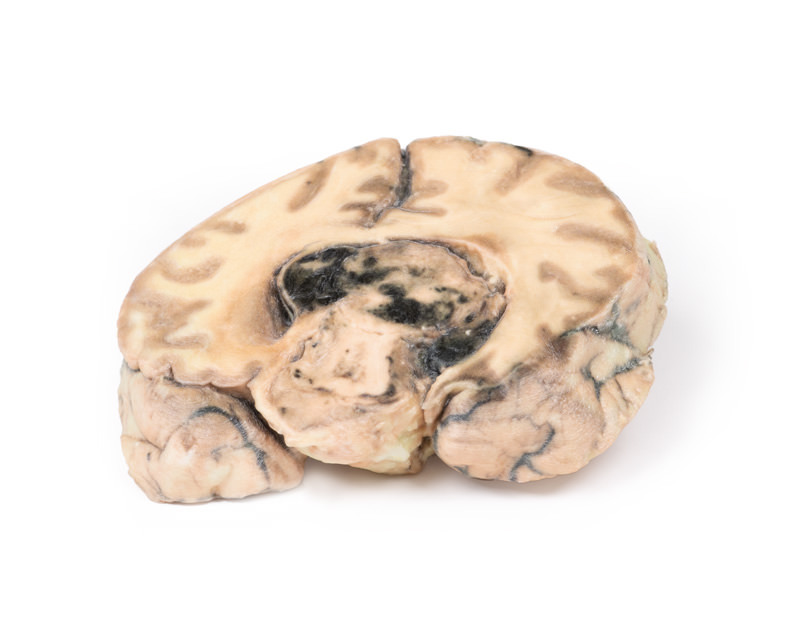
MP2016 - Glioblastoma multiforme